Restorative Care vs Dentures | Impact of Dentures on Health
By Shelby Tatomir on April 11, 2019 in Dental Health

Tooth loss used to be inevitable. Today, advances in technology and dental care allow us to keep our teeth longer than our ancestors ever did. But, longer-lasting, natural teeth means more risk for tooth decay. Dental caries or cavities is the leading cause of tooth loss in the United States today. If you or someone you love is missing teeth, consider the impact of dentures and restorative care on older adults. Make a fully-educated decision on your oral health or the oral health of a loved one.
Other factors also influence tooth loss in older adults:
Comorbid diseases – “Comorbidity” is a medical term for when a person experiences one or more conditions (physically, mentally, or behaviorally) that are caused by a primary health condition.
For example, 49 percent of individuals with arthritis also have heart disease, making them comorbid conditions. In oral health, dementia and tooth decay are “comorbid conditions.”
Chronic oral disease – A “chronic oral disease” is a condition that impacts your mouth over a long period. One of Delta Dental of Iowa’s goals is to stop common chronic oral diseases like periodontal disease.
Increased lifespan – The current lifespan for an individual is 72 years. That’s a full decade longer than the life expectancy the World Health Organization recorded in 2000. We expect our teeth to last a decade longer, as well. As our life expectancy increases, so does the importance of consistent preventive care so that we can enjoy healthy, natural teeth as we age.
Access to care - Complex issues affect access to dental care. This includes geography, finances, social-economic factors, pressing health needs, language barriers, and more.
Bridges, dentures, and implants are our current solutions to tooth loss. When tooth loss occurs, it’s important we look into alternatives. Individuals with missing teeth consume less protein, fiber, calcium, and vitamins. This is because tooth loss leads people to avoid certain types of foods that are harder to chew like fresh fruit, raw veggies, proteins, and other crunchy foods.
These individuals have a higher risk of obesity, diabetes, cardiovascular disease, and some cancers. Additionally, they are at risk for frailty from weight loss, especially later in life.
Dental Bridges – Are They Right for You?
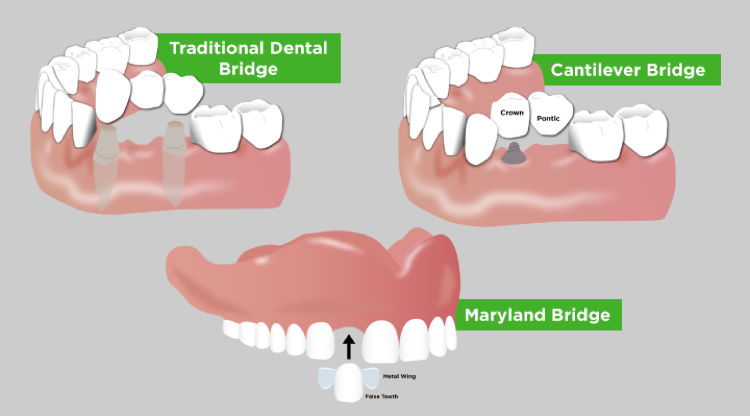
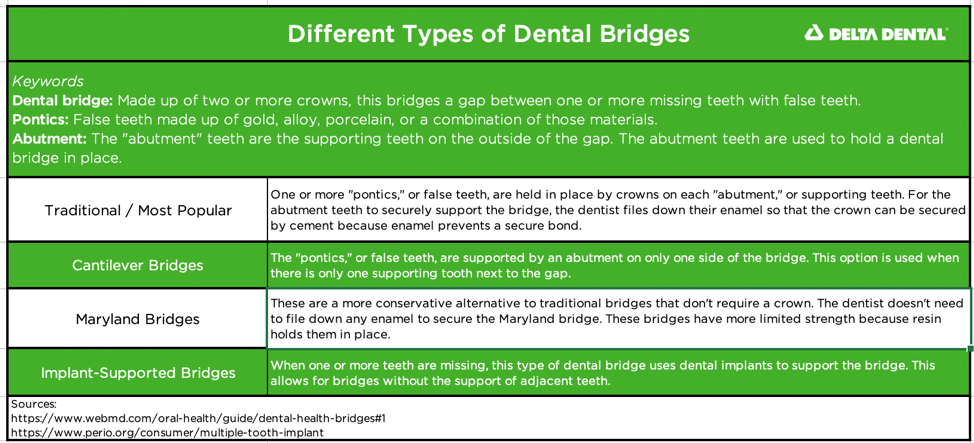
Dental bridges bridge a gap of one or more missing teeth. A dental bridge is made up of two or more crowns on either side of the gap. A crown is a tooth-shaped cap that is secured to a compromised tooth. It can help protect a sensitive tooth from further decay or help support its structure. When a dental bridge is constructed, crowns are usually placed on the teeth that sit on each side of the gap. The bridge uses the crowns to stay in place. Learn about traditional dental bridges, Cantilever dental bridges, Maryland dental bridges, and implant-supported dental bridges below.
If you or someone you love has experienced complete tooth loss, dentures may be a more appropriate option for restoring a smile than bridges.
Dentures and their Impact on Oral and Overall Health
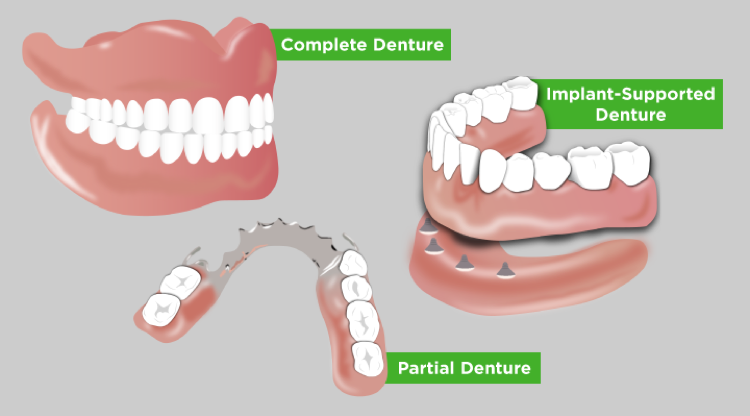
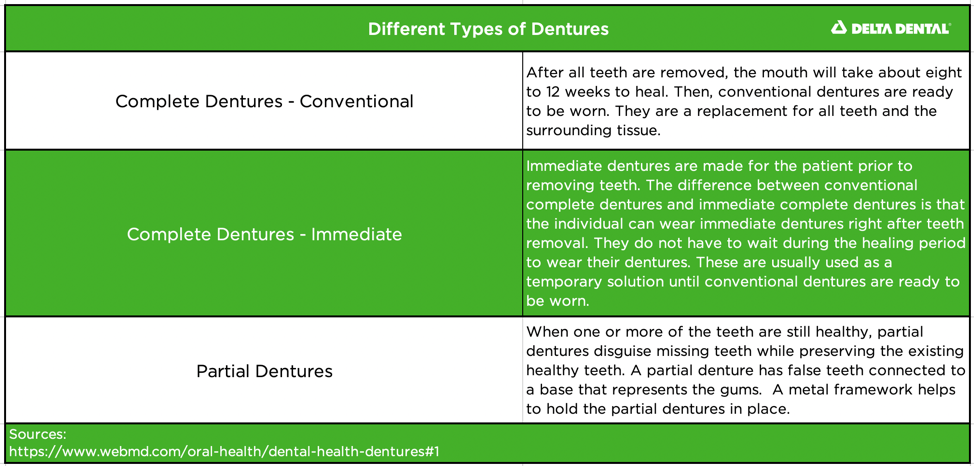
Dentures are made up of a false gumline and teeth that disguise tooth loss in a person’s smile. Dentures can make a significant impact on improving your overall health if they are the right choice for you.
“What positive impacts do dentures have on older adults’ quality of life?”
Eating, speaking, smiling all involve our teeth. When we lose our teeth, these activities can become cumbersome, challenging, and even painful. Dentures allow individuals without a full set of teeth to chew, eat, and speak more easily. Dentures can resolve malnutrition when accompanied by proper education around diet, too.
Dentures also increase an individual’s quality of life. Tooth loss is linked with a lower quality of life. In 2012, researchers discovered that older adults felt accomplished when they were able to care for their natural teeth. They experienced “a sense of achievement, pride, a sense of control, intactness, oral function, and comfort.” A natural smile has been connected with increased self-esteem and positive body-image. Conversely, tooth loss has been correlated with personality traits like aggression and stress.
“Are Dentures Right for Me?”
Denture wearers must commit to caring for their dentures every day. They need healthy gums and good oral hygiene practices. If intellectual or motor impairment get in the way of oral hygiene, dentures may not be the right choice.
Develop a strong understanding of the connection between what you eat, your smile health, and your overall health. Denture wearers should follow a healthy diet, too. Dentures help improve overall health by allowing the wearer to chew fruits and vegetables more easily. But, education around diet is as important as their new teeth.
Studies have shown that replacing missing teeth is not enough to improve an individual’s nutritional status. Nutrition and diet counseling inform them about how their oral health and diet are impacting their overall wellness.
Tooth grinding, or bruxism, is common in older adults and can result in the damaging of a dental appliance. Bridges, dentures, and other appliances are at risk of breaking if the wearer is a teeth-grinder. There is no cure for teeth grinding. Dentists often recommend the use of a night guard to protect teeth and enamel from the destructive habit.
“What negative impacts do dentures have on older adults’ quality of life?”
Some researchers are challenging the idea that all missing teeth should be replaced. Partial dentures are linked to serious increases in a person’s tooth decay index. People with partial dentures are six times more likely to develop tooth decay than patients with cantilever bridges. In this particular study, both groups received preventive care annually for five years. Yet, the group with removable partial dentures still had substantially more tooth decay.
Since our mouth shifts and moves over time, dentures also require maintenance and tailoring. If full dentures fit improperly, they can cause mouth sores. Partial dentures that fit improperly can cause decay, gingivitis, plaque build-up, and loss of supporting teeth. The older a pair of dentures are, the higher the wearer’s risk is for gingivitis, plaque build-up, and loss of supporting teeth.
Daily Denture Care for Older Adults
Dentures are fragile and should be handled with care.
- Remove dentures to brush at least twice a day and after each meal.
- Use denture cleaner or denture toothpaste to brush.
- Never use a harsh or abrasive cleaner as they may scratch the surface.
- Never boil dentures as it could cause them to warp and no longer fit
- Remove dentures for at least eight hours a day. This allows the gum tissue to rest. Then, the tongue and saliva can perform their normal gum stimulation and cleansing.
- To maintain a proper fit, adjustments or a set of new dentures may be needed after a few years.
Replace dentures every five years or as your dentist recommends. When in doubt, if something doesn’t feel right about your dentures, consult a dentist.
Restorative Care for Older Adults
Preventive care is the daily maintenance we do to keep up our oral health. When our preventive dental care isn’t good, tooth decay occurs, and it causes us to need restorative care. Restorative care includes fillings, crowns, implants, and more.
Older adults have different considerations than children or young adults when it comes to restorative care. Our skills for maintaining our wellness break down with age. If at-home or professional care is not available, their heavily-restored smile may begin to deteriorate. Other factors such as dry mouth (xerostomia) become more prevalent in the aging population. This can lead to a high risk for cavities and the need to replace existing restorations.
Older adults, if retired, generally have a fixed income. Restorative procedures can be costly and need maintenance and repairs. Say someone gets restorative care, such as dental implants at the age of 75. By their 80s, they may not have the financial or physical ability to handle and resolve a deteriorating dental situation.
Restorative Care and What’s Right for You
Ultimately, the choice to get dentures or other restorative care later in life should be decided on a case-by-case basis. If you, or someone you love, experiences cavities or decay as an older adult, ensure proper smile health care is taken. Brushing for two minutes in the morning and two minutes at night with an electric toothbrush is very effective. Don’t forget to combine with once-a-day-flossing for maintaining a healthy mouth!
Additionally, if you, or someone you love, is facing complications with oral health as an older adult, speak with a dental care provider. You can ask your dentist about popular solutions if dry mouth or salivation is a problem. Topical fluorides, remineralizing products, and xylitol chewing gum can help with dry mouth, as well as cavities.
For more information about the right next step in your dental care, talk with your dentist.
Don’t have dental benefits? You may not need to wait for the next open enrollment period. Find the dental plan that meets your needs today.
Time to find a dentist? Search and locate one close to you today.
Still need more info about dentures and other teeth replacement options? CLICK HERE to read more