Cosmetic Dental Procedures Classified: What Cosmetic Dentistry Means for Your Insurance
By Shelby Tatomir on July 25, 2017 in Insurance
From teeth whitening to getting braces and bridges, how does your coverage work when it’s classified as cosmetic dentistry?
Here’s a breakdown of the basics:
First things first. The American Dental Association (ADA) defines cosmetic dentistry work as: “Services provided by dentists solely to improve the appearance.” These treatments are for making the smile look better. The ADA definition goes on to say that procedures are classified as cosmetic when “form and function are satisfactory and no pathologic conditions exist.”
In other words, for a dental procedure to be considered cosmetic, it must only address appearance. If the patient needs the dental procedure to help with eating or speaking, for example, then it’s generally classified as a restorative procedure. That’s because restorative care will restore the mouth so that it’s functioning properly once again. On the other hand, cosmetic dental procedures, like cosmetic makeup, exist to change the way the mouth looks.
At Delta Dental of Iowa, we emphasize preventive dental coverage and share in the costs of other procedures. As part of this structure, your dental insurance usually covers:
Be aware that a deductible — the amount you pay before your dental insurance kicks in — may apply to these services, although it is usually waived for preventive and diagnostic services.
It’s important to note that coverage for cosmetic dental procedures like teeth whitening may not be covered by employer plans and are rarely covered by any type of dental insurance. This is because cosmetic procedures don’t improve oral or overall health and wellness.
3 Common Types of Cosmetic Procedures
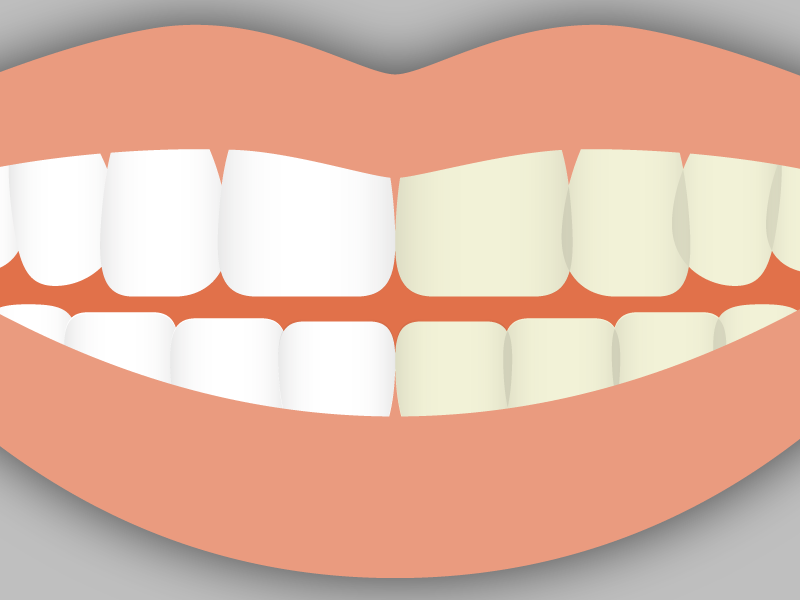
Teeth Whitening: Over 80 percent of Americans polled stated that they want to have whiter teeth. Teeth whitening is one of the most popular cosmetic dental procedures. If at-home whitening isn’t for you, you may look into teeth whitening at the dentist. In-office whitening treatments use peroxide and lasers. This treatment is effective, but it is more expensive than at-home kits.
Braces: Braces are a very common type of cosmetic dental procedure. They correct the alignment of our upper and lower teeth. This procedure is usually done with children, but braces are also used to correct crooked teeth, overbites, and underbites among people of all ages.
Coverage for braces falls under the orthodontic coverage category. The amount of coverage offered for braces will depend on your specific plan design. While it differs from plan to plan, some dental insurance may not cover select procedures such as orthodontia.
- Child Braces: Braces are usually recommended for children aged 8 to 14. The earlier in life that this cosmetic treatment begins, the better chance it has to give the patient the best smile possible because younger mouths are easier to adjust.
Click here to log into your online account and review your plan’s orthodontic coverage.
Dental Veneers: a veneer is a thin covering made to mask discolorations, brighten teeth, and generally improve the smile. When people have teeth that are discolored or damaged, dental veneers can be a popular choice. People often choose veneers over dentures, as they don’t need to be removed to be cleaned. The two options with dental veneers are composite or porcelain.
- Composite: A composite dental veneer uses a tooth-colored filling material to bond to the tooth. Usually, this procedure can be done in one dental visit and will cost less than porcelain veneers.
- Porcelain: This type of dental veneer has better stain resistance than composite veneers and better mimics the light-reflecting properties of natural teeth.
If you are interested in cosmetic procedures, contact your dentist to review your available options. Click here to find a dentist near you.
If you are hoping to schedule a cosmetic procedure, it is important to talk to your dental insurance provider before going through with treatment. Cosmetic procedures usually are not covered, but sometimes these procedures can be offered as optional in your benefits.
Already have a Delta Dental plan? Check out your dental plan specifics in the member connection today. Looking for dental coverage? Click here to shop for family or individual dental plans.
For more information on dental insurance, check out:
*Updated 2019